By Christina Wall, The Dying Year Team In the last several months I have had the privilege of sitting alongside several caregivers from early on in their loved one’s end-of-life process through time of death and beyond. I learn so much every time. Every circumstance is different. Every soup of family dynamics has its own flavor. How each person, the dying person and those who love them, approaches this transition seems to be such a poignant illustration of each unique personality. With those who have been fiercely independent, death often seems to come suddenly…as if they fought as hard and long as they could, then collapse and die within days. Those who have had a gentle approach to life, well, often seem to die…gently. Caregivers who desperately want control often struggle with the lack of control that comes with end-of-life. Those who have always been go-with-the-flow types often approach the unpredictable flow of the dying process with curiosity and awe. All of this and all the opposites of this too.
But I have narrowed down a constant in the last few months. Those who fair best in these times do their due diligence in planning while simultaneously embracing the truth that not a single plan may play out. I have sat with clients as they made pro/con lists, phone calls, delegated, designated, arranged spaces, made arrangements, etc.. And then I’ve sat with them in their frustration, sadness and often humor when none of those things logistically mattered because something unforeseen popped up along the journey. I say “logistically mattered” because it seems like there can be something emotionally important and significant in this planning process; something that has value beyond whether or not the plans work out. People really have the need to feel like they gave their “best” to these end-of-life situations and concrete planning helps meet that need. I strongly encourage it. But the most touching moments are those when I get to witness a client’s surrender to the natural course of things…when the control and desperation subside and acceptance fills the void. And with acceptance comes cleared space to be more present. What will hospice say during their visit today? I’m tired of guessing and researching. But I do know that I want to watch the sunrise with my momma this morning. When they say she’ll pass in “24-48 hours” which hour will it be? I don’t know. No one knows. But I do know that I can breath with her until she stops and soak in her essence in this remaining time. This is not to criticize the questioning and the turning over of all the stones. Lord knows I did so much of that myself in my own situation with my parents at their end-of-life. I had to go through it to get to the other side. I had to do my due diligence and have so many things not go as planned to understand how to be more present in their death. And so I sit and hold space for my clients on their own journeys. We make lists and phone calls together and then share tears and sometimes laughter when the plans of all those efforts fall apart. Then I sit with them as we build it all back up again simply by learning how to be fully present in the unpredictability of this precious transitional time. Your presence is enough my End-of-Life Warriors. Christina, End-of-Life Doula, The Dying Year Team
0 Comments
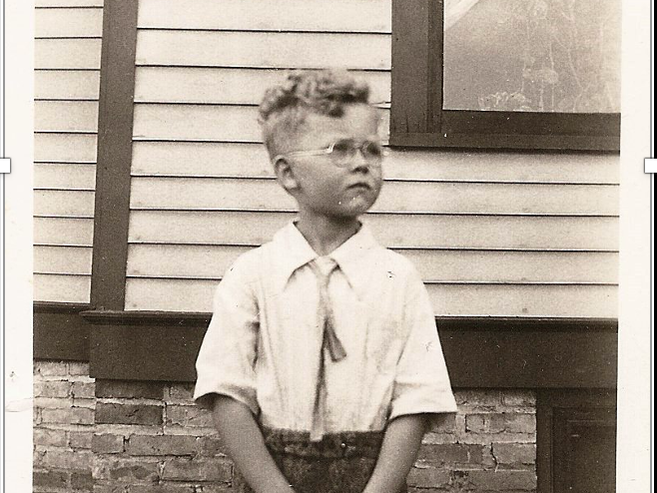
My dad died one year ago February 9. In preparation for this important milestone, I knew I had to do something special. As I prepared for it I was overwhelmed with feelings and knew that I needed help. I remembered that a recent EOL doula student had done a lot of work around her dad’s relationship with his mother, who died young. My grandmother died at age 26. My dad had mentioned that he wanted to be buried near her. So, I planned to take some of his ashes to the cemetery. This led to so much more emotional work about my grandmother and their brief relationship.
My dad never talked about his mother. We didn't call her grandmother. There were no photos and the story was very fuzzy. He would answer questions, but I had to ask. All this is part of my legacy, stuff I'm trying to figure out. My dad was raised by his maternal grandparents and great-grandparents. His parents divorced in 1933 and his mother died suddenly in 1935 when he was just five. I found myself thinking so much more about what he went through, and why we didn’t talk about it, and how this affected us all. I wanted to know more about her story. Fortunately, I found some old letters that she wrote that filled in a lot of info, some of it very tragic. I'm going very deep, and I'm not sure where this is leading. I continue to identify that I am grieving. I feel very new at grief. It's kind of foreign to me. We don't talk about this in my family (my legacy?). I'm pretty much alone. Or am I? Funny, I have studied this, I teach about this, I support others in doing this. Yet, it's been so difficult for me. I've had to learn to ask for help, slow down, be with it. I'm thankful for the student who ended up being my doula and going with me to the cemetery. She helped me create a ceremony. I also have my family and other people to reach out to, a supportive partner, and the time and luxury to be able to go inward. It's been a very interesting year so far. I'm on a journey. We are always on a journey. Sometimes the path is a little scary. ***** Merilynne He died five months ago. This morning I lit a yellow candle, played Roy Orbison (one of his favorites), and thought about him. How happy his mother must have been when he was born! His was not an easy childhood. His parents divorced when he was two and his mother died when he was five. Being raised by his grandparents and great-grandparents was no picnic. But he grew into a loving man and was a pretty good dad to me.
Today I tried talking to him for the first time since his death. That doesn’t come naturally to me for some reason (even though I regularly talk to friends who have gone before). Mostly I just thank God for him, for his long life, and for all he gave me. This is my first big, long grief journey. Here is what I’ve learned so far:
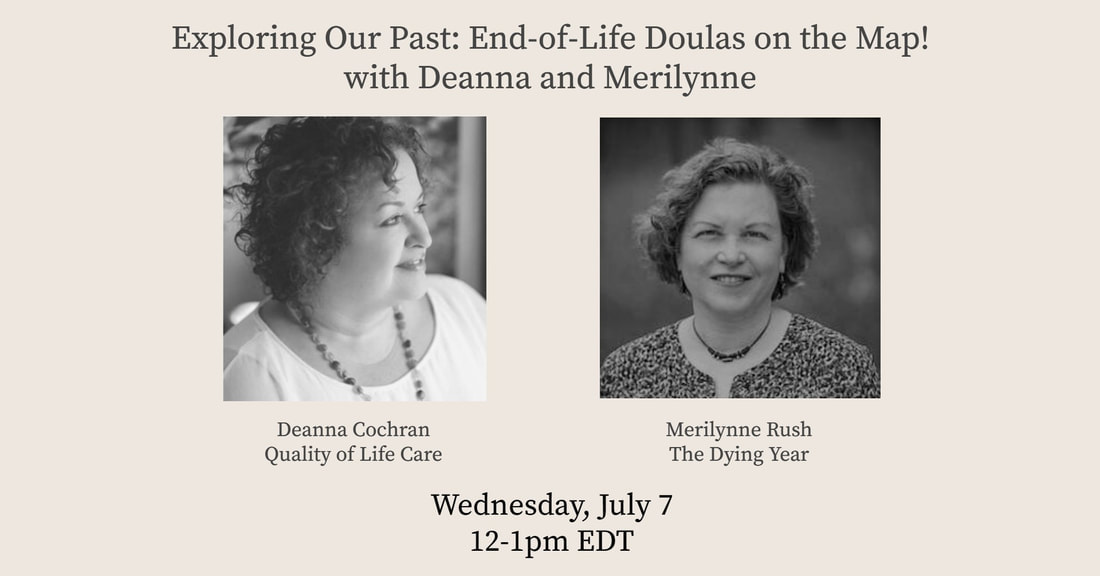
Deanna and I have been friends for a long time. Wet met when I asked her if I could share some of her educational materials with my students. Wow! What a powerhouse she is! We instantly hit it off and began networking and sharing ideas about this work, supporting each other as innovators and teachers. As I was talking with Deanna I realized the benefits of coming together with other leaders in this field to learn from each other and further our work. That's the kind of person we both are: the more the merrier :) In early 2017 we began planning what we called the "End-of-life Doula Network." Later that year, as Deanna put together a meeting with the NHPCO leadership, our Network morphed into the National End-of-life Doula Alliance, and we invited everyone we could think of who was teaching at the time to join us.
That's the story of my beginnings with Deanna. But her history with EOL doula work goes back much further. She is going to share with us what she knows. People, mostly women, have been caring for their dying loved ones forever. It is what people do. We live and die in community (most of us) and we care for each other. Throughout herstory the role has been given many names as certain people were identified as having special experience, knowledge or skills in this area and were called upon again and again. We honor those who have come before us in all traditions and what they have passed down to us. We invite you to think about who has influenced, taught, or inspired you to be involved in this work. We recognize that only recently have we separated out this role from other caregiving work and given it a new name. We celebrate the many threads that grow out of all traditions and cultures. In this webinar we take the time to name those who come before us, known and unknown. Together we will move forward, weave it all together, and bring our services to those who need them. Won't you join us as we explore our past, stand strong in our present, and dream about our future? To join the live webinar on July 7, please register here. New course, fully online with LIVE virtual office hours begins October 18, 2021!
I'm thrilled to offer this completely revamped training, in collaboration with Brian Hayden and Redesigning the End. Individual modules include reading, viewing, writing exercises, and other exciting activities to prepare you to guide others in caring for their own dead at home. Home funeral, fully legal in all 50 states, is a natural way to continue loving death care in the home, with no need for the body to go to a funeral home. Ideal for those who have been in hospice care and who embrace a natural approach that is environmentally friendly. I have been teaching about natural death care since 2009 and have assisted over 50 families having a home funeral. Ideal for end-of-life doulas, funeral professionals, spiritual care providers, and hospice workers, the curriculum includes history of US funeral practices, legal considerations, state-by-state laws, benefits of home care, how to care for the body, supplies, special circumstances, creating a ceremony or gathering, anatomical donation and much more. Students are fully prepared to take the National Home Funeral Alliance (NHFA) Proficiency Exam and earn their Badge. This class is offered in collaboration with Redesigning the End. For more information and to register, click here. Cost: $595. Questions? Contact Merilynne.  Sometimes life is an uphill struggle. What gets you through? Substances Work Faith Screentime/videos/tv Family Community Meditation Yoga Exercise Be honest! Some days were good this winter, some not so good. Now its springtime and I'm looking ahead - I have a chance to reinvent myself. Which of these things will help me brighten my future?
I am so glad we decided to have an online virtual memorial gathering soon after my father’s death. It brought us together as siblings and gave us something to do during those first days and weeks after he died. It was difficult and it took a lot of work. It was distracting. After it was all over there was a let down and I felt my grief more deeply and in different ways than I did leading up to the memorial. But it gave us so many benefits — we shared our memories, created a beautiful 7-minute slide show, met with old friends and family far and wide, and we have a recording of the whole gathering that we can cherish. If we hadn’t done this at this time, I don’t think we would have done anything in the future when we can gather in person again. Or at least it would have been different, and perhaps more difficult. It is satisfying and comforting to look back on this gathering now, even though it had to be online.
The inspiration and model for this came from the “zoomeral” of my partner’s aunt. The first thing I did was tell my siblings about that experience and how beautiful and helpful it was. I called the organizer of that event to ask about the details – super helpful!! I had planning meetings on zoom with my siblings — this gave them an opportunity to get more comfortable with that platform. Our event took place about 2 ½ weeks after my dad died. It was a bit of a scramble, but we didn’t want to wait too long and it was worth it. I think there is a lot of value in doing it soon to give you something to work toward, to express your feelings while they are still very fresh, to give others a chance to participate and come together, and to get past it so you can focus on other things and other ways of grieving. We kept it short; it’s difficult to be on zoom for very long, and we wanted kids to be able to be there. Fewer transitions between speakers, photos and music means less potential for technical glitches. We had some prayers, about 5-10 minutes of music, a 7-minute slideshow with music, personal sharing from the children of the deceased for 15 minutes, and about 15 minutes of open sharing. An additional wonderful feature was having breakout rooms after the formal gathering for further discussion among friends and family. We hired a zoom technical assistant to:
You also need an MC for the event. My recommendation is that it be someone close to the family, but not an immediate family member. The MC is the primary speaker who is the leader, welcomes everyone, sets the tone, states the purpose of the event, keeps things on track, invites others to speak, and closes the event. In our case, the MC was also the pastor who led the prayers at the beginning and end. Other things we did:
Biggest lessons learned:
I hope this information helps anyone planning to do a virtual memorial. Other resources: Steven Birenbaum, How to Hold. Virtual Memorial Service, NYT 1-14-21 https://www.nytimes.com/2021/01/14/well/family/virtual-funeral-advice.html Debbie Waldman, How to Pay Your Respects During a Virtual Funeral, Wired, 3-17-21 https://www.wired.com/story/zoom-funeral-etiquette-manners/  There are no cue cards, there is no rule book. I only have the bits and pieces of what I have learned from other people’s stories, from books or movies, from a class. I have to write my own story, I have to figure this out for myself; I have to design my own plan. I have to walk this journey in my own shoes, no one to guide me. It’s like flexing a new muscle, developing a new skill; one I always knew I would have to learn, one you can’t really prepare for, something I knew lurked ahead but ... Now I have jumped off this cliff. I come from a very productive-oriented life: Work Do Solve Fix Make. With producing things there is a sense that, if you just do it right, it will work. Put in the time, follow the directions, get the right tools, make it work; use your problem solving skills. With this grief, there is no … It is different; it is not a problem to be solved with my mind. It takes time, but another kind of time. Time to just be, to feel. I almost have to get sick to slow down and feel, be with my memories. This is a different kind of work; one I am not as good at. It feels weird, ungrounded, unhinged, new. This is where I can rely on what I have heard, what I have learned from others’ experiences: This is normal. I have to keep telling myself that. It is ok to just sit. In fact, it is necessary. My dad died February 9, 2021. All that I have learned and talked about for so many years helped me to be at his bedside and be fully present with his dying and my grieving. I want to share a few lessons that I learned on this journey. Thank you for listening, and for your compassion.
 Dad and Sarah, activities director Dad and Sarah, activities director My dad lives in a facility and is dying of dementia. Each week I look at him on a screen. He is being taken care of by caring, young (mostly) women. I am so grateful for them and the love they give him. Some of them are activities directors, some are aides. They each have their individual job description, but a lot of what they do overlaps, especially now during Covid-time. All hands are on deck to be with the residents of assisted living facilities because family, and others, can’t be there. My father’s aide tells me she is spending as much time as possible with the residents. The aides and others know that they are the heart and hands of the family and loved ones right now and they focus even more on providing companionship, touch, humor, love, and so much more. There are other roles that overlap with caring for people at end-of-life: fixer/handyperson, therapeutic pet care person, meal deliverer, housekeeper… the list goes on and on. The longer someone works in a caring profession, the more they learn by experience about end-of-life. But many of them do not have specific training about specific areas of end-of-life care like the dying process, grief and bereavement (including their own), life review, comfort touch, vigil-ing, community resources, advocacy, advance care planning, and funeral options. That is why so many people are attracted to the end-of-life doula role. The doula learns about and addresses all of these areas. The doula does not replace the other roles; doulas add another layer of support, spend time, focus on companionship, and collaborate with all care providers. Doula-ing is all around us, it is not new. It takes many people in all of our capacities to care for each other. The doula concept brings it all together under one title, but others are still needed. We all need each other. Doulas bring everything they have and everything they are to the work. Doulas are changing end-of-life care. |
|
Speak with Merilynne about |
Find A TRAINING for |
find resources |
Website designed by Lee Webster, Side Effects Publishing
|
MAKE A DONATION to support the work of The Dying Year that helps other just starting out in the end of life doula field. Thank you!







 RSS Feed
RSS Feed


